Scoliosis Vs Multiple Sclerosis may seem like unrelated conditions. However, they share a common thread - the silent struggles they bring to those affected. Scoliosis is a curvature of the spine. It can cause physical discomfort and self-consciousness while Multiple Sclerosis¹, an autoimmune disease, silently attacks the central nervous system, leading to a range of debilitating
symptoms. Understanding these conditions is essential for advocacy and support. In this article, we will delve into the complexities of Scoliosis vs Multiple Sclerosis, shedding light on the challenges faced by those living with these conditions.
Understanding Scoliosis: Causes, Symptoms, And Diagnosis

Scoliosis, a spinal deformity², is found in children aged 10 - 18. This can also manifest in adults primarily as idiopathic, degenerative, or neuromuscular types. Idiopathic scoliosis evolves from adolescence, unnoticed until adulthood. Degenerative scoliosis stems from the spine's age-related degenerative changes. In contrast, neuromuscular scoliosis is tied to conditions causing muscle or nerve impairments, often leading to asymmetric weakness. Though not directly linked to scoliosis, the immune system is pivotal in overall health, influencing scoliosis progression and healing, particularly after surgery. Enhanced understanding and support of immune health are crucial in adult scoliosis care, aiding in managing symptoms, addressing spinal deformity, and optimizing postoperative recovery.
A. Causes
1. Idiopathic Scoliosis
Idiopathic scoliosis, accounting for about 80% of cases, manifests without a clear underlying cause. It typically emerges during the adolescent growth spurt and can progress as the individual grows. Despite extensive research, the exact cause remains unknown, but genetic aspects are believed to play a role. While most idiopathic scoliosis cases are mild³, some can progress and may require intervention.
2. Congenital Scoliosis
Congenital scoliosis⁴, results from abnormalities in the vertebrae present at birth. These anomalies can disrupt normal spinal development, leading to curvature. This type varies widely in severity, and its management depends on the extent of the malformation.
3. Neuromuscular Scoliosis
Underlying disorders like Cerebral palsy, Myelodysplasia, Spinal muscular atrophy, and Friedrich ataxia can develop neuromuscular scoliosis⁵, affecting muscle tone and control, leading to the development of scoliosis, which is an abnormal curve of the entire spine (Gurd & Badve, 2020, pp. 159-161).
4. Degenerative Scoliosis
Adults can develop scoliosis because of tumors, multiple sclerosis, or other problems. Degenerative scoliosis⁶ is typically associated with the natural aging process and degeneration of spinal structures. As discs and joints deteriorate, the spine may develop an abnormal curve. This type is often accompanied by back pain and can progress gradually. Treatment may involve pain management, physical therapy, and, in some cases, surgery to stabilize and correct the curve. (Kotwa et al., 2011)
B. Symptoms
Uneven Shoulders or Hips
Individuals with scoliosis may exhibit unevenness in the height of their shoulders or hip dips. This asymmetry is a result of the lateral curve of the spine, causing a noticeable tilt in the body's alignment. Depending on the severity of the curve, these uneven features may become more pronounced over time.
Spinal Curve
A hallmark symptom of scoliosis is the presence of a sideways curvature in the spine when viewed from the front or back. This deviation from the normal spinal alignment can range from mild to severe and may progress as a person grows. The degree of curvature is typically measured using the Cobb angle on X-rays.
Uneven Waist
Scoliosis can lead to an uneven waistline, where one side appears higher or more prominent than the other. This visual asymmetry is a consequence of the spinal curvature affecting the alignment of the pelvis and the distribution of body weight.
Tilted Head
In some cases, individuals with scoliosis may exhibit a head tilt, where the head is not centered directly above the pelvis. This tilt can compensate for the spinal curvature as the body adjusts to maintain balance and alignment.
Back Pain
While not always present, scoliosis can be associated with back pain or discomfort, particularly in cases where the curvature is more severe. The pain may result from muscle imbalances, pressure on nerves, or the strain on the spine due to the abnormal curvature.
C. Diagnosis
1. Physical Examination
During a physical examination, a healthcare professional conducts a thorough assessment of the patient's posture, gait, and body symmetry. They look for visual cues such as shoulder height discrepancies, waist irregularities, and other signs of spinal curvature.
2. Imaging Tests

Common scoliosis diagnostic imaging includes X-rays for spinal alignment and, occasionally, MRI or CT scans for spinal cord and nerve evaluation. These methods detect scoliosis early, measure it precisely, and facilitate effective treatment planning, ensuring proper care for patients.
D. Treatment
1. Observation
To manage symptoms for mild cases of scoliosis, especially in growing children and adolescents, a common approach is to monitor the condition through regular check-ups. Observation allows healthcare professionals to track the progression of the curvature and intervene if necessary as the individual continues to grow.
2. Bracing

In moderate cases where the curvature is at risk of progression, a brace may be prescribed. Bracing aims to prevent further curvature during the period of skeletal growth. The type and duration of bracing depend on factors such as the degree of curvature, skeletal maturity, and the specific characteristics of the scoliosis.
3. Surgery
In severe cases or when other interventions prove ineffective, surgical intervention may be recommended. Spinal fusion surgery aims to straighten the spine and prevent further curvature progression. During the procedure, metal rods and screws are often used to stabilize the spine, and bone grafts encourage the fusion of the vertebrae.
Early diagnosis and prompt intervention are key in managing scoliosis effectively. Regular screenings, especially during periods of rapid growth, enable timely identification and appropriate management, ultimately improving outcomes and the individual's quality of life. If there are concerns or symptoms suggestive of scoliosis, seeking prompt evaluation by a healthcare professional is essential.
Understanding Multiple Sclerosis: Causes, Symptoms, And Diagnosis
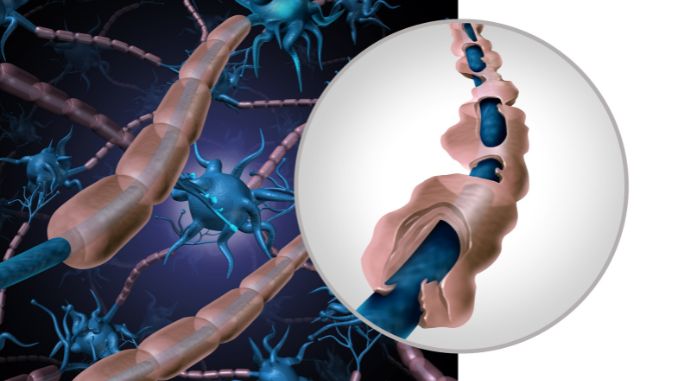
MS is an autoimmune disease⁷ that mistakenly attacks the protective covering of nerve fibers (myelin sheath), leading to inflammation and damage. This disrupts the normal flow of electrical impulses along the nerves and can result in a wide range of symptoms, including new symptoms and sometimes affecting sexual function⁸ (Severson, 2024).
A. Causes
Scientists aren't sure what exactly triggers multiple sclerosis, but they believe genes and environment likely play a role.
Certain genes may increase susceptibility to the disease. Environmental factors, such as viral infections or low vitamin D levels, may trigger the immune response leading to the development of MS⁹. It is considered a complex interplay of genetic predisposition and environmental triggers.
While Multiple Sclerosis (MS) itself doesn't cause scoliosis, it can lead to a condition called secondary scoliosis in adults over many years. This happens because MS weakens muscles and ligaments around the spine unevenly. This weakness, combined with wear-and-tear changes in the spine's joints (arthritis), can cause the spine to curve abnormally. The nerve damage from MS is permanent and gets worse over time
B. Symptoms
Difficulty Walking
MS frequently affects coordination and balance, resulting in challenges with walking. Individuals may experience stumbling, weakness, or a lack of coordination, making mobility a significant concern
Numbness or Tingling
Sensations of numbness or tingling, medically referred to as paresthesias, common in an MS patient and can occur in various parts of the body, including the face and limbs. These sensory disturbances are indicative of nerve involvement.
Muscle Weakness
Muscle weakness is a prevalent symptom in MS, affecting both the upper and lower extremities. This weakness can vary in severity and may contribute to difficulties with daily activities.
Dizziness and Vertigo
Some individuals with MS experience dizziness or vertigo, often accompanied by a spinning sensation. These symptoms can be disruptive and impact balance and overall well-being.
Emotional Changes
The emotional effect of living with a chronic condition like MS is profound. Mood swings, depression, and anxiety can occur, influenced by both the physical effects of the disease on the central nervous system and the emotional challenges of managing a chronic illness.
C. Diagnosis
1. Medical History and Physical Examination
Establishing a diagnosis of Multiple Sclerosis begins with a comprehensive medical history and a thorough neurological examination. Healthcare professionals assess symptoms, their duration, and any patterns indicative of central nervous system involvement.
2. MRI (Magnetic Resonance Imaging)

MRI plays a pivotal role in diagnosing MS by revealing areas of demyelination, inflammation, and scarring in the brain and spinal cord. The detailed images obtained aid in confirming the presence of lesions characteristic of MS.
3. Lumbar Puncture (Spinal Tap)
A lumbar puncture may be executed to analyze cerebrospinal fluid for specific markers associated with MS. Elevated levels of immunoglobulin G (IgG) or the presence of oligoclonal bands can support the diagnosis.
4. Evoked Potential Tests
Evoked possible tests measure the electrical activity in the brain in response to stimuli, helping identify abnormal nerve conduction. These tests can provide additional evidence of central nervous system involvement in MS.
5. Blood Tests

While there is no exact blood test for MS, general blood tests may be conducted to rule out other conditions with similar symptoms and to assess overall health.
D. Treatment
1. Disease-Modifying Therapies (DMTs)
Disease-modifying therapies (DMTs) are a cornerstone of MS treatment. These medications act on the underlying disease process to reduce the number and intensity of relapses, as well as slowing down the progression of disability.
2. Physical and Occupational Therapy
Rehabilitation programs, including physical and occupational therapy, is crucial in managing MS. These programs focus on maintaining or improving mobility, strength, and overall functional independence.
3. Lifestyle Modifications
Adopting a healthy lifestyle is integral to MS management. Stress management, balanced diet, and regular exercise, and contribute to overall well-being and can positively influence symptom management.
Takeaway In Scoliosis Vs Multiple Sclerosis
In the face of scoliosis vs multiple sclerosis challenges, individuals exhibit remarkable resilience. Despite distinct musculoskeletal and neurological issues, hope unites them. Medical advancements, adaptive strategies, and support fuel their optimism.
Scoliosis Vs Multiple Sclerosis both conditions can impact quality of life, they are fundamentally different in terms of their underlying mechanisms and the systems they affect.
Each day showcases their courage as they manage symptoms, adapt, and pursue fulfilling lives. Through determination, those with these conditions inspire not only themselves but also others, proving that life can thrive amidst health challenges. Both scoliosis vs multiple sclerosis involve the spine, they are distinct conditions with different causes and treatments.
There is a comprehensive, yet simple to follow program that contains the exercises you need to know to recover from lumbar spinal fusion surgery.
Check out our Lumbar Spinal Fusion Recovery Program just for you!








